
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.


 Insurance Suitability form (PDF) - Blue Cross and Blue Shield of . " width="208" height="300" />
Insurance Suitability form (PDF) - Blue Cross and Blue Shield of . " width="208" height="300" />








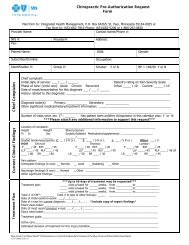
PROVIDER CLAIM ADJUSTMENT / STATUS CHECK / APPEAL FORMBlue Cross Blue Shield of Minnesota and Blue PlusOne form per request or appeal.Indicate the number of related requests/appeals being submitted for the same member. Specify ____ of ____ (e.g., 1 of 5).Today’s Date: _______________________Contact Person:________________________________________ Phone _____________________ Fax ______________________BCBSMN Tax ID or Provider ID:_______________________ NPI: __________________Provider Name: _____________________________Provider Return Address:BCBSMN Member ID#:Patient Name:__________________________________________________________________________________________Claim #:□Blue CardPlan Code __________Group #:Patient Account:Charge for service in question:Service Date(s) in question:Claim Adjustment Request/Status CheckA claim adjustment request is based upon a correction and/or newinformation for a previously processed claim. Adjustment requests are notappeals. We can not adjust claims to deviate from contract benefits.For Status Check: Please check Provider Web Self Service or call Provider Services. Please wait 30 days from the date you submittedthe claim before checking on the status.Enter the remark codeCOMMENTS: ___________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Other Carrier Paid (include EOB – Explanation of Benefits)Medicare (include EOMB)No-Fault auto insuranceWorkers’ Compensation_____________________________________________________Appeal (Attach supporting documentation – Please refer to theProvider Policy and Procedure Manual for instructions)An appeal is a request for reconsideration of a previously processedservice (denial, payment reduction, coverage termination, etc.)Enter remark codeCOMMENTS: ______________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________Website: http://www.bluecrossmn.com click on ‘For Health Care Providers’ for the Provider Policy & Procedure Manual,Forms: OtherMail to: Blue Cross Blue Shield of Minnesota FAX to: 651-662-2745Attn: Appeals or Claim Adjustments Attn: Appeals or Claim AdjustmentsPO Box 64560St Paul, MN 55164-0560Form X16156R05 (01/09)